Locals drive deep DNA tech
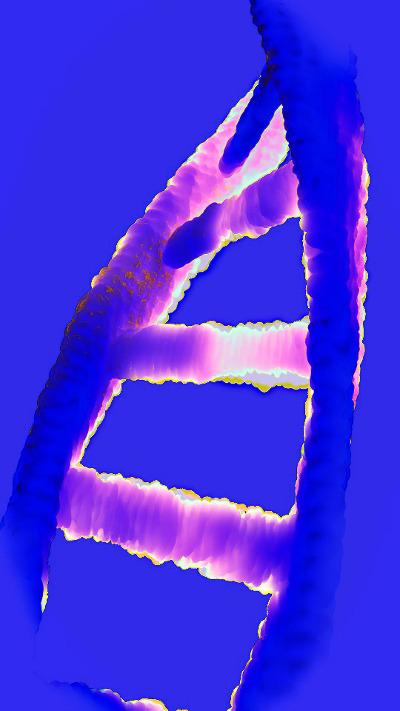 Australians are pioneering a powerful new genome editing technique.
Australians are pioneering a powerful new genome editing technique.
The technology can activate any gene – including those that have been silenced – allowing new drug targets and causes of drug resistance to be explored on an unmatched level.
In tests so far, researchers have leveraged the unique technology to replicate an aggressive form of lymphoma for the first time, which they used to identify a gene responsible for triggering drug resistance to a new treatment for blood cancers.
Lymphoma is the most common blood cancer in Australia, with around 6,500 Australians diagnosed each year.
Double hit lymphoma (DHL) is an aggressive subtype that affects white blood cells called B lymphocytes, or B cells.
In a first, a team from the Walter and Eliza Hall Institute of Medical Research (WEHI) has enhanced a genome editing technology, known as CRISPR activation, to accurately mimic DHL.
Project lead Professor Marco Herold said the team focused on DHL as the disease is difficult to treat, in part due to a lack of efficient pre-clinical modelling.
“Without the ability to model a disease, there are limited opportunities to properly test which drugs will be effective for it in the clinic,” said Professor Herold, who established and now leads one of Australia’s most advanced CRISPR laboratories at WEHI.
“The technology is a game-changer for the scientific community and people in the clinic as it allows us to mimic diseases like DHL and properly test drug treatments against them for the first time.
“This is significant when you think of the plethora of human diseases that could be better modelled by using this tool.”
Venetoclax is an anti-cancer drug based on a discovery made at WEHI in the late 1980s - that a protein called BCL-2 helps cancer cells survive indefinitely.
A1 is a pro-survival protein of the BCL-2 family. Activation of this gene has been reported in diverse forms of cancer, including leukaemia, lymphoma, melanoma, stomach cancer and breast cancer.
While A1 had been thought to play an important role during cancer progression, PhD student and first author, Yexuan Deng, said this had remained unverified – until now.
“As DHL lymphomas from our model can be killed with venetoclax, we were able to leverage this to prove for the first time that A1 is a major factor in resistance to this drug,” Deng said.
While cancers are often triggered by switching genes on, researchers have largely only been able to switch them off in previous disease models.
Project lead Associate Professor Gemma Kelly said the team was able to engineer drug resistance because their model can activate any gene – even those that have been silenced.
“We used this model’s unprecedented ability to switch on A1, which allowed us to confirm the protein as a resistance driver,” Associate Professor Kelly said.
“Our research will allow for more genes to be activated in other models to better understand cancer drivers and, critically, to determine other causes of drug resistance.”
The research has sparked international interest, with the WEHI team working with researchers from Nanjing University (China) and Genentech (US), a member of the Roche Group, to develop the technology.
The findings are published in Nature Communications.







 Print
Print